When Pfizer initially released its COVID-19 mRNA vaccine, distributing it was a major challenge. Scientists thought that the vaccine had to be stored at -70°C, requiring dry ice or ultra-cold freezers. At scale, explains David Lewandowski, Azenta’s Strategic Partnerships Manager for Automated Storage, “Temperature matters. The warmer it is, the easier it is [to deliver medicines].” This hurdle was eventually solved by additional testing that showed the doses could be stored safely in standard freezers for a couple of weeks. “For cell therapy, we don’t have that option [at this time].”
Delivering cell therapies is a cold, complicated affair
Living cells are inherently more complicated than conventional drugs or RNA therapies. They cannot survive for long once removed from the human body. Extremely cold temperatures are needed to preserve them, as practically every biochemical process ceases below the glass transition temperature of water (around -135°C). Storage within a liquid nitrogen freezer (at -190°C) prevents cell damage but severely complicates the manufacturing and distribution of cell and gene therapies. Cryogenically frozen cells must remain safely below -135°C. Even brief warming events – such as those caused by someone reaching into a freezer and taking out racks — can endanger cell viability and function.
No two cell therapies are alike, and different types of cells vary considerably in their composition and metabolism, requiring highly customized cryopreservation processes. Each new treatment demands a complex and unique process for storing and transporting the cells. These novel logistical demands create unavoidable inefficiencies in product development and commercialization. As more cell therapies come to market, manufacturers and clinicians will struggle to keep up.
Standardization to the rescue?
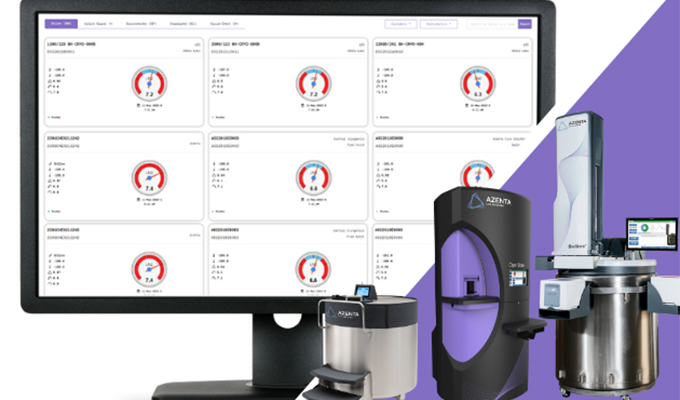
Infrastructural limitations have spurred the industry to push for standardization. Even standardizing something as seemingly insignificant as product packaging can be surprisingly beneficial. For instance, with a single container size, a liquid nitrogen freezer can be packed more efficiently. Technicians are better accustomed to handling the materials, which reduces human error. And, importantly, uniform packaging makes automated storage much more feasible – which further improves product quality and streamlines tracking. All of which are critical in a world where a million dollars’ worth of work can be destroyed in seconds if a lab tech takes too long getting materials out of a freezer.
Unfortunately, the ability to automate and standardize is limited. Attempting to create a one-size-fits-all process is doomed to failure. “Depending on your cells, depending on your targets, depending on your mechanism… everything changes. So even though people want standards in this cryopreservation process, standards would be very hard to achieve with so much variation between products today,” says Lewandowski.
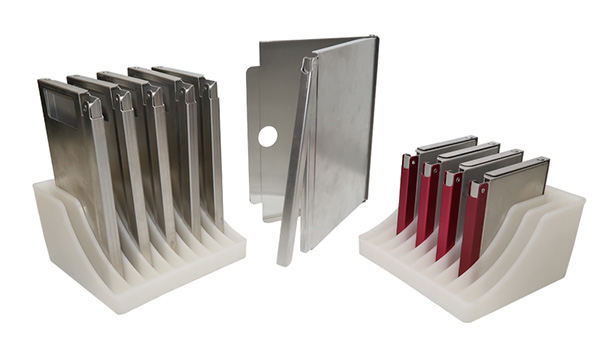
This doesn’t mean that there are no targets for standardization. A lot of industry attention is currently focused on packaging. At the time of writing, there are no standards for the packaging of cell therapy products. Bags, vials, and cassettes (the aluminum frames that encase bags during freezing and storage) come in a wide range of shapes and sizes. This poses an immediate problem on the patient side. Places like the Moffitt Cancer Center in Tampa, Florida, are undertaking dozens of cell therapy trials, and products are stored in a range of container types, shapes, and sizes depending on the company. This creates complexities in storing, handling, and managing inventories at the clinic. “Consistent storage and cold chain infrastructure will make it easier for everyone including the clinic doing the important handling and patient coordination,” explains Lewandowski.
Automated storage systems designed to work with multiple formats can help deliver flexibility. The recently launched CryoArc™ Pico is one example.
The industry begins to move
At the Cryo Symposium for Cell & Gene Therapy, where the need for standards was a recurring theme, Dr. Rui Li from West Pharmaceutical Services polled the audience about the about standardization during her talk entitled “Cryogenic Packaging (R)Evolution 2022-2032.” A “limited selection of unified outer dimensions” for packaging was the single most desired improvement for distribution and clinical hubs. The sentiment was echoed at a discussion session hosted by Dr. Dawn Henke from the Standards Coordinating Body for Regenerative Medicine and Lexi Garcia from the Advanced Regenerative Manufacturing Institute. Attendees overwhelmingly chose secondary containment (e.g., the dimensions of cassettes) as the highest priority for standardization. This is a concrete problem that is explicit and solvable, and the will is there to address it.
Momentum is building and the industry is rallying — if not yet around a specific standard — then behind the need to establish said standard. Nonprofit organizations like the Standards Coordinating Body are bringing together relevant stakeholders to formulate and recommend solutions. A working group of the International Standards Organization (ISO) Technical Committee 276 on Biotechnology will meet later this year to draft “general requirements for the design of packaging” for cell therapies. “The world will benefit from [the industry] working together,” says Lewandowski, “and there are good signs of excellent representation and participation across the industry.”
The recorded talks from the inaugural Cryo Symposium for Cell & Gene Therapy featured presentations about current advances in cryopreservation and key considerations for cold-chain management of advanced therapies. You can access them below.